A Renewed Focus on Simulation and Procedural Excellence
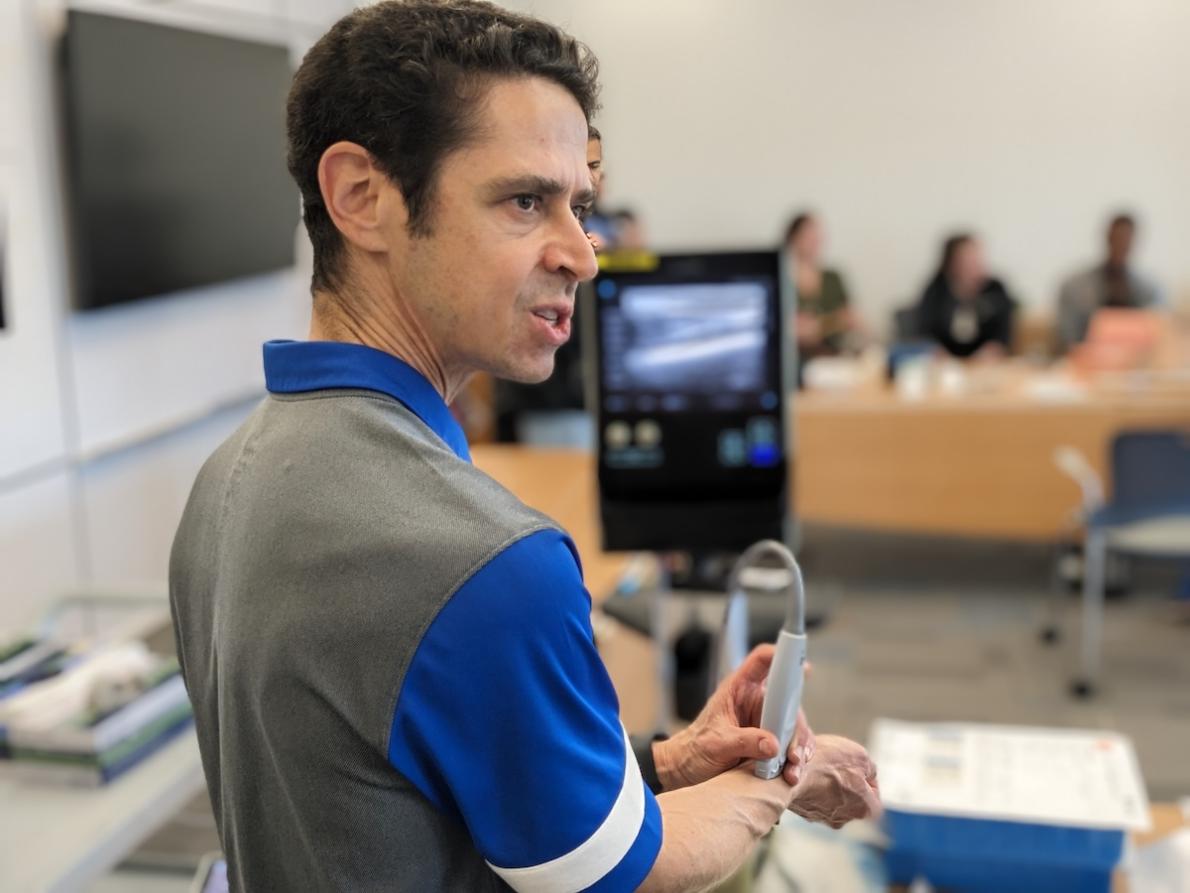
The Duke Emergency Medicine Residency has placed renewed focus on simulation and procedural excellence. The program provides five hours of monthly simulation to residents, including task training and high-fidelity team-based resuscitations.
During the 2023–24 academic year, the program invested substantially in new resources and personnel for the simulation program. Jessica Robertson, DO, took on a new role as Core Faculty for Procedures, joining Cathleen Bury, MD, Director of Simulation, in leading education in these important domains. The program acquired an advanced transvenous pacemaker insertion model, allowing trainees to practice a high stakes, rare, invasive procedure.
The Department also purchased a pericardiocentesis simulator that allows ultrasound-guided access through the traditional subxiphoid approach, and also via a more recently described parasternal window. For peritonsillar abscess drainage, the program worked with Duke School of Engineering students to develop a model, as no commercially available solution exists. And the program is developing a Colles fracture reduction model with engineer David Mercer, part of an initiative to increase procedures performed by Emergency Medicine residents and enhance the appropriateness of consultations.
Following sessions for residents, the program offered training to faculty, which have been well-attended. “It’s important for us to harmonize the skills we’re teaching residents in simulation with the clinical practices of our faculty. It’s great to see faculty committing themselves to lifelong learning and keeping their knowledge on the cutting edge,” says Program Director and Vice Chair of Education Josh Broder. “I’m excited by the number of occasions in which residents reached out to say they’ve had the opportunity to do a procedure successfully as a direct consequence of the training we’ve provided to them and our faculty. Patients are benefiting from safer, more effective, and more timely procedures.”
Next steps for the program include creating care pathways to standardize approaches to procedures and research to better characterize the patient and trainee-oriented benefits of simulation. “Sim isn’t a ‘nice to have’ — it’s an essential part of our safety and quality system,” says Broder.
Dr. Robertson and Dr. Bury are rolling out new initiatives for orthopedic care, integrated with the simulation program. They envision QI projects assessing the frequency of orthopedic consultation, patient length of stay, and procedure rates for a range of common orthopedic injuries. The program will be working again with the School of Engineering this fall, mentoring freshmen students in the project-based introductory course, EGR 101. This also creates a natural opportunity for residents to engage in research to assess the effectiveness of new simulation tools and techniques.
As the Residency continues to evolve its training, the Department is also expanding its offerings to the world beyond Duke. Operational and clinical improvements, scholarly activity, and CME courses all will go hand in hand. The Department will host a CME simulation-based procedure course on September 13, with 16 faculty participating as instructors.