The Duke University School of Medicine Department of Emergency Medicine held its first external continuing medical education (CME) course on September 13, 2024, at the Trent Semans Center for Medical Education. The event showcased critical medical procedures, taught by expert Duke EM faculty using high-fidelity simulators. The course was months in planning.
The curriculum committee conducted a needs assessment by surveying residency graduates to identify high-yield topics. Participants visited from North Carolina, Massachusetts, New York, Virginia, and Illinois. The course earned a 5-star rating from attendees: “Great mix of high-yield didactics and lots of hands on.” “All instructors were knowledgeable, small groups allowed for lots of practice, models were high fidelity.”
Transvenous Pacemaker Simulation
At the transvenous pacemaker station, participants learned about appropriate settings for a transvenous pacing device, pearls and pitfalls of a transvenous pacing electrode and catheter kit and practiced inserting a real catheter and electrically capturing using a MedTronic pacemaker and a SimuLab PacerMan. Station faculty included Associate Residency Director Dr. Sreeja Natesan and Kami Arulraja, who recently completed critical care fellowship at Duke after serving as Emergency Medicine Chief Resident.
Surgical Airway
The surgical airway station reviewed essential anatomy and steps in surgical airway, using both a high-fidelity manikin and tissue. Participants learned to use readily available emergency department equipment such as a bougie and endotracheal tube, as well as practicing the use of more specialized tools such as a tracheal hook, Trousseau dilator, and Weitlaner retractor. Faculty for the station included Dr. Ken Kennedy.

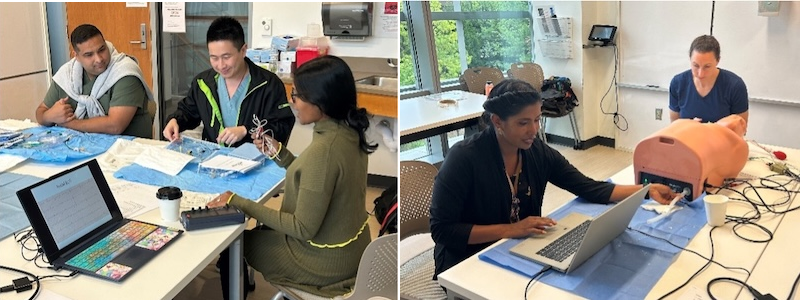
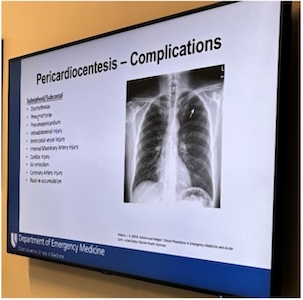
Pericardiocentesis
Attendees practiced identifying a pericardial effusion using a Vimedix ultrasound simulator, followed by performing three approaches for ultrasound-guided pericardiocentesis in a model. Simulation Director Dr. Cathleen Bury, Duke LifeFlight Assistant Director Dr. JJ Hoff, and Dr. Jessica Robertson led the station.
Advanced Cardiac Ultrasound
At the advanced point-of-care ultrasound station, participants practiced specialized exams under the direction of three fellowship-trained Duke ultrasound faculty, two of whom have also earned the Focused Practice Designation (FPD) in Advanced Emergency Medicine Ultrasonography (AEMUS), a certification from the American Board of Emergency Medicine (ABEM). Participants used both a high-fidelity Vimedix cardiac ultrasound simulator and actual ultrasound equipment to scan instructors. Instructors included Dr. Tim Peterson, Dr. Shawn Sethi, and Dr. Brandon Ruderman.
Paracentesis/Thoracentesis
The thoracentesis and paracentesis station allowed attendees to use ultrasound guidance to identify fluid collections and avoid internal organs in high-fidelity models, as well as to familiarize themselves with specialized catheters including Seldingertechnique and trocar-guided pigtails. Faculty members Dr. Erin Leiman, Dr. Aubree Anderson, Dr. Samuel Francis, and Dr. Tim Peterson provided participants with expert-level training.

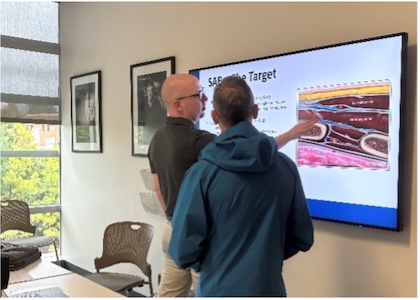
Nerve Block
Attendees also had unique opportunities to learn ultrasound-guided regional nerve blocks using a blend of tissue and synthetic materials. Instructors Dr. Kevin Gurysh and Dr. Christopher Nash taught fascia iliaca, erector spinae, and serratus anterior plane, useful for pain management in hip fracture, chest wall trauma, and chest and abdominal trauma, respectively. Dr. Gurysh created nerve block models from scratch utilizing yarn, JP drains, and lots and lots of meat. Dr. Nash created 3D-printed bony anatomy, overlaid with tissue. Participants noted the station’s applicability, with one noting that nerve blocks were “something I feel like I hadn’t really learned before but are very doable and I can immediately put into my practice.”

Peritonsillar Abscess
Under the guidance of Duke faculty Dr. Megan Rivera and Dr. Jessica Wanthal, participants reviewed CT scans of peritonsillar abscess and performed peritonsillar abscess drainage using 3D printed models designed and built
specifically for the course by Dr. Christopher Nash and Dr. Josh Broder.

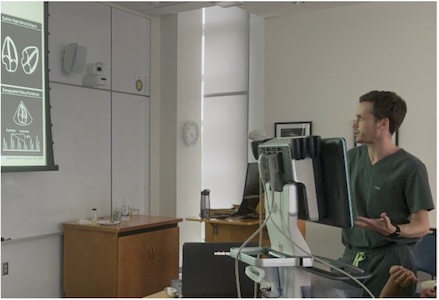
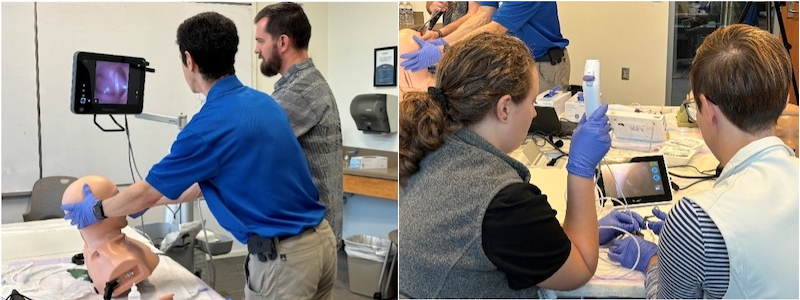
Flexible Laryngoscopy
Participants practiced nasal and oral flexible laryngoscopy and intubation in pediatric and adult airway manikins. The station highlighted airway anesthesia, scope controls and navigation, and performing the procedure with a patient in both supine
and upright positions. As a bonus, participants practiced removal of ear foreign bodies using both flexible scopes and small Bluetooth-connected cameras with a smartphone.
With the success of the course, the Department is planning for future events. Participants praised the course and faculty:
“Blocks, transvenous pacing, and laryngoscopy are very useful and also having muscle memory, time to troubleshoot in a low-key environment was so important and helpful. “
“The 3D printed models for peritonsillar abscess drainage were really neat and helpful. Was also impressed with the usage of the meat for nerve block practice! It was much more lifelike and thus especially useful.”
“Nerve block, was really well taught and seem very applicable. Something I feel like I hadn’t really learned before but is very doable and I can immediately put into my practice.”