At Duke, resident training is aimed at developing outstanding clinical, research, and leadership skills through clinical rotations and educational programs.
Our residency curriculum covers the core content of emergency medicine as well as cutting-edge emerging evidence for new diagnostic and therapeutic approaches.
Residents in the Department of Emergency Medicine at Duke have access to numerous clinical and research opportunities to prepare them for independent practice.
PGY-1
| Rotation | Weeks |
|---|---|
| ED | 21 |
| PEM | 4 |
| Resuscitation | 4 |
| US/Anesthesia | 4 |
| Gen Med | 3 |
| Cardiac ICU | 4 |
| OBGYN (L&D) | 4 |
| VA ED | 4 |
| Vacation | 4 |
PGY-2
| Rotation | Weeks |
|---|---|
| ED | 20 |
| PEM | 4 |
| Community ED | 4 |
| ED Nights | 4 |
| EMS | 2 |
| ED Ortho | 2 |
| MICU | 4 |
| SICU | 4 |
| PICU | 4 |
| Vacation | 4 |
PGY-3
| Rotation | Weeks |
|---|---|
| ED | 26 |
| PEM | 8 |
| Resuscitation | 4 |
| ED Nights | 4 |
| Elective | 4 |
| LifeFlight/Admin | 2 |
| Vacation | 4 |
The Duke Pediatric Emergency Department is a quaternary care, level 1 trauma center focused on providing outstanding care to all pediatric patients as well as their families. Our team includes 13 fellowship-trained, board-certified Pediatric Emergency Medicine (PEM) physicians, ensuring 24/7 full-time PEM faculty coverage. Residents spend 5 months of their training focused on the care of pediatric patients, 4 months in the ED, and 1 month in the PICU. The rotations intentionally include both focused (e.g., 2 weeks at a time) and longitudinal elements (e.g., intermittent shifts throughout the years).
As a tertiary referral center, Duke offers residents unparalleled exposure to medically complex and critically injured infants and children, with access to the full range of pediatric subspecialties for consultation. Residents gain critical experience caring for patients with congenital heart disease, adrenal insufficiency, ventriculoperitoneal shunt complications, respiratory failure, multiple organ transplants, complex oncological conditions and treatments, multi-trauma exposure as well as patients needing ECMO cannulation and therapy. Additionally, residents quickly gain expertise with common pediatric complaints and procedures, while developing the skill to recognize and treat common conditions in medically complex children. Through experience in the pediatric emergency department, curated off-service rotations, and high-fidelity simulation, the Duke Emergency Medicine Residency Program ensures crucial training in pediatric intubation as well as low-frequency high-risk procedures. This combination produces graduates who are highly skilled in the comprehensive emergency care of infants and children.
Our faculty are recognized for excellence in education and service, with honors including the Golden Apple Award (the highest teaching award from Duke medical students), the Master Teacher/Clinician Award, and multiple Department of Pediatrics Divisional Teaching Awards.
Current areas of active research in the pediatric emergency department include patient safety, bronchiolitis outcomes, national pediatric sedation initiatives, internet-based teaching innovations, and collaborative projects across divisions, such as novel RSV treatments and improving care for neonates with fever.
We are honored to have the opportunity to teach residents the critical skills needed to expertly care for sick and injured children. The Duke pediatric emergency department is an excellent training environment for those seeking a well-rounded, robust education in preparation for emergency care of infants and children in any setting post-residency.
Airway management is central to emergency medicine, and Duke Emergency Medicine residents receive the best possible training. In our simulation lab, realistic airway mannequins allow residents to experience a range of airway anatomy with an array of equipment. Our residents train in surgical airway techniques using percutaneous kits and surgical techniques, in both high fidelity mannequins and tissue models. Our simulation lab also features hyper-realistic bronchoscopy simulators, allowing residents to safely master flexible fiberoptic techniques for difficult airways. In our department, residents use the Karl-Storz CMAC video system, allowing training in direct as well as video-assisted laryngoscopy.
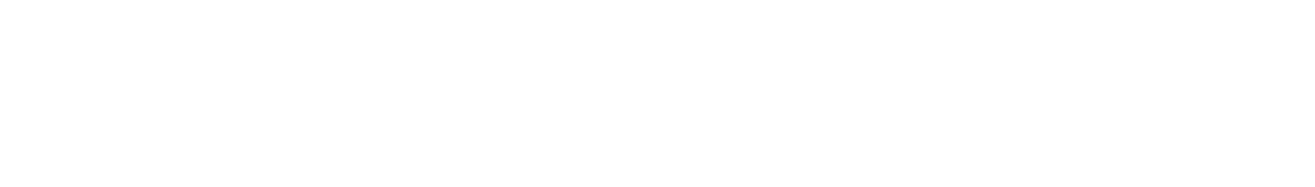
Simulation is deeply integrated into the Duke Emergency Medicine residency curriculum, with a dedicated conference day each month focused on procedures and the resuscitation of both pediatric and adult patients in our advanced simulation center.
Since 2013, our state-of-the-art center has been located in the Mary Duke Biddle Trent Semans Center for Health Education, providing a realistic, multi-bed emergency department environment where residents can hone their skills.
Our center features a wide array of high-fidelity tools and technology designed to deliver immersive, hands-on training:
- Adult and pediatric high-fidelity mannequins for resuscitation and procedural practice
- Modern ultrasound machines and simulators (Vimedix, SonoSim, Sonosite) for point-of-care ultrasound skills
- Central line trainers (subclavian, IJ, femoral) compatible with real-time ultrasound guidance
- Airway task trainers and models for cricothyrotomy, needle decompression, and advanced airway management
- Trauma procedure trainers for chest tubes, pericardiocentesis, and IV cutdown
- Lumbar puncture and vascular access task trainers
- Tissue lab to further expand procedural experience
We are also proud to incorporate home-grown simulation models—many developed in-house using 3D printing—for a variety of emergency procedures. Recent innovations include models for distal radius fracture reduction, peritonsillar abscess drainage, ultrasound-guided nerve blocks and more, allowing residents to develop hands-on expertise with emerging techniques.
Simulation resources are incorporated not only into conference days, but also throughout the resuscitation rotation during the first and third years and the longitudinal ultrasound curriculum. These opportunities help ensure that Duke EM residents graduate with confidence and competence in high-stakes clinical scenarios.
About the Simulation Director
Christopher J. Nash, MD, EdM, completed Emergency Medicine residency at Massachusetts General Hospital/Brigham and Women’s Hospital (MGH/BWH) from 2017–2021, followed by a medical education fellowship at MGH from 2021–2023. After returning to Duke—where he completed his undergraduate studies—he joined the faculty in 2023, became Core Faculty in 2024, and was appointed Simulation Director in 2025. He brings a passion for innovation in simulation and a strong commitment to advancing emergency medicine education at Duke.
Emergency ultrasound at Duke University Medical Center is integral to providing the best possible clinical patient care, resident and student education, and innovative research endeavors in emergency medicine.
With 10 ultrasound machines in the Emergency Department (two Sonosite PXs, two GE Venues, two Sonosite M-Turbos, one Sonosite Edge, three Sonosite S-nerves, and multiple handheld Butterfly IQ units for educational use), a full-time director of Emergency Ultrasound, 5 additional fellowship-trained ultrasound faculty, and a high-fidelity ultrasound simulator in our state-of-the-art simulation center, the EM residency provides the best in cutting-edge training.
All PGY-1 residents have four total dedicated weeks for ultrasound education and training during their first year of residency to master the fundamentals of clinical ultrasound. They receive subscriptions to both the Core Ultrasound fundamentals course and QBank for asynchronous learning and learn directly from our ultrasound faculty during one-on-one scanning sessions and weekly image review. Senior residents may use additional elective time to learn advanced ultrasound techniques and further their training, and all residents have monthly small-group hands-on training during ultrasound workshops on sim day.
Ultrasound Director Erica Peethumnongsin, MD, PHD
I trained at the University of Wisconsin - Madison Emergency Medicine Residency program and became interested in ultrasound through mentorship from great educators in the field. I recognized during my training how bedside ultrasound can rapidly change a patient's entire clinical course, particularly when resources are limited. After residency, I completed a fellowship in emergency ultrasound at the Georgetown/Washington Hospital Center program and am committed to using the knowledge and skills I acquired to improve patient care and resident education here at Duke. 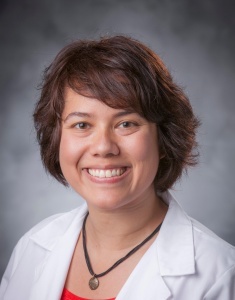
Since 2013, the Duke Emergency Medicine Residency Program has invested in high-fidelity ultrasound simulation systems to help residents learn image acquisition and interpretation during their rotations and sim day sessions. The Vimedix simulator, shown below, provides a standardized model for practice scanning with the added advantage that learners can explore various pathological findings that require rapid management and occur rarely in practice, such as pericardial tamponade, ventricular fibrillation, or aortic dissection.
Technology that keeps track of how your smartphone is oriented can now give $50,000 ultrasound machines many of the 3-D imaging abilities of their $250,000 counterparts — for the cost of a $10 microchip.
Below, the Vimedix simulator provides additional hands-on training and a range of pathology for Emergency Medicine residents.
Learn more about simulators at Duke.
"How a $10 Microchip Turns 2-D Ultrasound Machines to 3-D Imaging Devices"
Technology that keeps track of how your smartphone is oriented can now give $50,000 ultrasound machines many of the 3-D imaging abilities of their $250,000 counterparts — for the cost of a $10 microchip.
Medical toxicology focuses on the diagnosis, management or prevention of poisonings. It encompasses a wide range of topics including: pharmaceutical misadventures, drugs of abuse, occupational exposures, envenomations and environmental exposures, radiation, and bioterrorism.
Duke Emergency Medicine has a long history of outstanding clinical care and scholarship in key areas of toxicology: dysbarism and disorders of dive-related supraphysiologic nitrogen absorption (learn more about the hyperbaric center at Duke), carbon monoxide poisoning, and snakebite. We are a leading center for a multicenter study of antivenin for copperhead snakebite, led by Charles Gerardo, MD.
Duke has a long and storied history in the specialty of Undersea and Hyperbaric Medicine. Learn more about our hyperbaric center and fellowship opportunities.


Durham County EMS
During their training, Duke Emergency Medicine residents have the opportunity to work in several aspects of prehospital care. Our residents primarily interact and rotate with Durham County EMS, the sole provider of emergency ambulance services in Durham County. Residents also have opportunities to ride along with Wake County EMS and provide education and training to nearby rural EMS systems.
The Durham County EMS system provides advanced life support paramedic ambulance service throughout the county as well as first responder support through the City of Durham Fire Department and three volunteer fire departments – Bahama, Lebanon, and Redwood. The system also encompasses the Durham Emergency Call Center, which is the primary safety answering point for all 9-1-1 calls within Durham County.
Durham County EMS also supports multiple special programs, such as the tactical emergency medical support (TEMS) unit which provides medical support to the Durham Police Selective Enforcement Team (SET), the Sheriff’s Emergency Response Team (SERT), and a CBRNE EMS unit that provides medical support to the Durham Police Department’s Biological-Chemical Emergency Response Team (B-CERT). Additionally, Durham County EMS has a robust Community Paramedic/Mobile Integrated Health division, supporting community members through innovative initiatives such as the Medication for Opioid Use Disorder program providing treatment through field inductions.
Dr. Anjni Joiner currently serves as the Medical Director with Dr. Erin Hanlin as Associate Medical Director. They are equipped with an ALS response vehicle equipped with additional equipment to allow them to perform physician-level interventions in the prehospital setting. Duke EM PGY2 and PGY3 residents, as well as faculty, serve as online medical control for Durham County EMS.
Emergency Preparedness and Disaster Management
Residents also have an opportunity to participate in emergency preparedness and disaster management activities. Dr. Erin Hanlin serves as the Medical Director for Emergency Preparedness for Duke University Hospital. Residents receive annual mass casualty incident training. Those with additional interest in Emergency Preparedness and Disaster Medicine can work with the Emergency Department mass casualty incident (MCI) Working group to take an active role in planning and preparing. Residents with a NC state medical license can also be members of the NC400 State Medical Assistance Team (SMAT), which is part of North Carolina's state-wide emergency response system. SMAT also covers multiple events throughout the Triangle Region, and interested residents can get experience in event medicine coverage alongside the SMAT.
Duke Life Flight
Duke Life Flight serves both the local region and beyond as a premier critical care transport agency, utilizing both air and ground vehicles to not only transport patients, but also provide excellent care. Frequently, Life Flight crews can be found transporting patients from smaller hospitals to the Duke Emergency Department for definitive care at a tertiary facility and Level 1 trauma center, as well as interfacing with EMS agencies to bring patients to Duke directly from the scene in cases of trauma, STEMI, and stroke. There is a deeply intertwined relationship between Duke Life Flight and Duke Emergency Medicine, not only in the realm of patient care on a daily basis, but also in clinical oversight and education. Duke EM faculty members Dr. Jason Theiling and Dr. JJ Hoff serve as Medical Director and Assistant Medical Director for Duke Life Flight, respectively.
In addition to critical care transport, Duke Life Flight also serves Duke Hospital through the Code Team, as well as the Duke and Durham community through its Event Medicine program. The Code Team responds to unexpected emergencies throughout the Duke Hospital Campus, frequently transporting these patients to the Duke Emergency Department for further care. The Event Medicine team provides medical coverage for major events on Duke’s campus, including sporting events, graduations, concerts, and other events with large gatherings of people. Under the medical direction of Dr. JJ Hoff, these highly-skilled teams can provide on-scene medical care to patients and coordinate transport to the Duke Emergency Department as needed.
Duke EM residents have the opportunity in their third year to rotate through the various aspects of Duke Life Flight as part of a required two-week rotation. During this rotation, they have the opportunity to participate in Air Transport if they choose, as well as Ground Transport, Code Team, and Event Medicine.
The strong relationship between Duke Life Flight and Duke Emergency Medicine allows for high-quality patient care to those in the Triangle region, but also to expand its reach beyond to more distant areas.

Medical student education is a major priority in our residency. Our residents routinely teach students in the emergency department and in classroom and simulation settings.
Associate Professor David Gordon, MD serves multiple key roles: Associate Residency Program Director for Emergency Medicine, President of the National Clerkship Directors in Emergency Medicine, and Medical Director for the Clinical Skills Lab, which teaches all Duke Medical Students the fundamentals of performing a history and physical exam. Dr. Gordon is a nationally recognized expert in cognitive errors in emergency medicine.
In this video, Dr. Gordon shares secrets to effective emergency medicine presentations for medical students.
Below, Chief Resident for the Duke Emergency Medicine Class of 2014 Scott Evans teaches medical student during a simulation activity, "Haunted ED." Dr. Gordon developed this concept and presented this as an educational innovation at the annual meeting of the Council of Residency Directors in Emergency Medicine in 2014.